Neisseria gonorrhoeae
- Etiology of Gonorrhea
- Greek (gonos – seed and rhoia- flow)
- First described in urethral discharge by Neisser in 1879
- Cultured by Bumm in 1985 and proved its pathogenecity by inoculating human volunteers
- Resemble meningococci very closely in many properties
Sample:
- Endocervical swab (not vaginal swabs)
- Uretheral discharge, urine (in males)
- Discharge after prosthetic massage,
- Conjunctival swab in case of opthalmia neonatrum
- – Throat infection may also occurs, in such case throat swab
- In DGI, specimen may include blood, swabs of skin lesions, urine
Sample collection
(A)Collection or urethral discharge from male:
- Cleanse around the urethral opening using a swab moistened with sterile physiological saline.
- Gently massage the urethra from downwards, using a swab, collect a sample of discharge.
- Make a smear of the discharge on a microscope slide by gently rolling the swab on slide which will avoid damaging pus cells that contain the bacteria.
- Note: Very few pus cells may be present if the patient has recently passed urine. Allow 2–4 hours after urination before collecting a specimen.
- When culture is indicated, collect a sample of pus on a sterile cotton-wool swab.
- To isolate from urine, early morning first voided urine sample is taken, centrifuge and take the sediments.
- A rectal swab is required in case of homosexual patients.
(B) Collection of cervical specimens from female
- Use a sterile vaginal speculum to examine the cervix and collect the specimen.
- Moisten the speculum with sterile warm water, and pass so that cervix could be visualized properly. Do not lubricate the speculum with a gel that may be bactericidal.
- Cleanse the cervix using a swab moistened with sterile physiological saline.
- Pass a sterile cotton-wool swab 20–30 mm into the endocervical canal and gently rotate the swab against the endocervical wall.
Transport media:
- Spot inoculation of sample on culture medium
If not possible,
- Specimens should be collected on charcoal impregnated swab
- –Transported to lab on Stuart’s transport medium
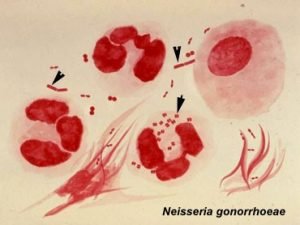
Gram Staining: Gram negative, bean shaped diplococcus, intracellular as well as extra cellular
- Characteristic intracellular gram negative diplococci lying with polymorphoinuclear leukocytes and few extracellular – positive
- Aprrox. 95 % infected male yield positive result
- Not reliable in women unless intracellular gram negative diplococci is seen as there are other bacteria with similar morpholgy which appear like Neisseria gonorrhoeae
Direct detection:
- Direct detection in patient secretion can be done which avoids problems with transport.
- Gonozyme test: polyclonal antibody test to detect gonococcal antigen by enzyme immunoassay.
- Direct florescence test
- Slide agglutination test
Culture the specimen
- Modified New York City (MNYC)
- Thayer Martin medium with VCN
- Chocolate agar
-Incubation at 37°C for 24 hour in a moist atmosphere containing 5-10% CO2 by placing a damp piece of filter paper at the bottom of the jar.
ADDITIONAL CULTURE
– Inoculate the specimen on two plates of Blood agar and incubate one anaerobically and the other aerobically at 35–37°C overnight.
Colony characteristics:
- small, round, translucent, convex colonies grow with finely granular surface after 24 hrs
- After 48 hrs, colonies are larger with crenated margin and opaque raised center
- On Thayer Martin medium, growth is slow
Kellogg divided gonococci into 4 types on the basis of coloial morphology, auto-agglutinability and virulence
Four types of colonies
– T1, T2: virulent and contains pilli, small brown colonies
– T3, T4: avirulent and nonpiliated, large granular, non pigmennted
-Test suspected colonies by touching with a cotton bud soaked in oxidase reagent, contact area of bud turns purple within 5-15 Secs.
Biochemical reaction
- Catalase ,Oxidase, Glucose: +ve
- Lactose, sucrose and maltose: -ve
Antibody detection in patients sera:
- Complement Fixation test (CFT)
Beta lactamase testing:
- Inoculate the medium with several colonies of organisms and place 6 microgram of penicilln disc on the well, if ZOI is less than 20 mm after overnight incubation, test for beta lactamase by chromogenic cephalosporin method
- -Nitocephin, a chromogenic cephalosporin is normally yellow and turns red when hydrolyzed.
- -Inoculate 50µl of heavy suspension of bacteria into the well of a microtitre plate and add 10µl of nitrocephin solution
- -Incubate 30 mins, observe for color change.
Sensitivity to physical and chemical agents
- Verile fragile organism
- Readily killed by drying, soap and water and many other cleaning or antiseptic agents
- May remain viable for a day in pus contaminating linen or fabrics
- Cutured gonococci dies in 3-4 days at room temperature
- Stored for several months by harvesting the isolate into 1 ml trypone soya broth containing 6% lactose at -20°C or -70°C
Pathogenesis
- Venereal disease transmitted by sexual contact
- Incubation peroiod – 2-8 days
- Confined to mucus secreting epithelial cells
- Pili mediates the adhesion og gonococci to the urethra or mucosal surface

- Cocci penetrates through the intercellular space and reach subepithelial connective tissue by the 3rd day after infection
- Penetrate columnar epithelial cells. Stratified squamous epithelium is resistant
- Attack mucous membrane of genitourinary tract, eye, rectum and throat producing acute suppuration followed by chronic inflammation and fibrosis
Disease in men
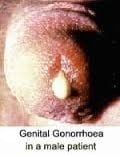
- Acute urethritis (most common clinical presentation in male few days after unprotected sexual intercourse)
- Dysuria and purulent penile discharge
- Infection may extend to prostate, seminal vessicle and epididymus
- Chronic urethritis may lead to stricture formation
- Infection may spread to periurethral tissue causing abcesses and multiple draining sinuses
Disease in woman
- Endocervix is the primary site of infection and extends to urethra and vagina giving rise to mucopurulent discharge

- Vaginal epithelium are resistant to infection in adults but severe vulvovaginitis may occur in prepubertal girls
- Asymptomatic carriage in woman is common (rare in man)
- Symtomatic patients commonly experience vaginal discharge, dysuria and abdominal pain
Non-gonococcal urethritis in men
- Chlamydia trachomatis is a common cause of non-gonococcal urethritis (NGU), particularly in men.
- A presumptive diagnosis of NGU can be made when a urethral smear contains 5 or more pus cells and no intracellular Gram negative diplococci (or more than 15 pus cells in a first voided urine specimen from a male patient).